COVID-19 is a microscopic virus, not fully alive. It’s a parasite, seeking hosts without discrimination. Flattening the curve of rapid spread, preventing it from overwhelming health care workers and systems that have inadequate supplies of personal protective equipment (PPE) and ventilators is a critical problem. Solving a specific part of this problem became job number one for an ER doctor and her husband, a mechanical and software engineer.
Sarah Farris, M.D., an emergency physician for the department of emergency medicine at Prisma Health, and assistant medical director for the Greenville HealthCare Simulation Center in Greenville, South Carolina, spoke with SWE Magazine about the invention process for an up-to-four-way ventilator splitter, now called VESper™.
Her husband, Ryan Farris, who has a B.S. in mechanical engineering from Michigan State University and now works as an independent software engineer, joined the conversation.
“The idea of the ventilator splitting is not new and is not my idea,” Dr. Farris said. “Historically, it’s been used during the Las Vegas, Nevada, mass shooting. An emergency physician taking care of the victims had published a paper in 2006 on a way to use existing respiratory air circuit parts to construct a ventilator splitter. When he heard of this shooting, with multiple victims coming in, he assembled a splitter because they had more critical patients than ventilators.
“As America started preparing for the COVID pandemic in late February and early March, there was discussion in my Facebook groups and with colleagues about how to handle the ventilator shortage,” she said. “As Italy began rationing ventilators because they had no other choice, I remembered the ventilator splitter option that several people had discussed. One of the problems of using preexisting pieces is that you need those pieces to fit the other parts of the ventilator circuit while anticipating shortages of equipment that would happen with a patient flood — PPE and medications and, obviously, ventilators. If we could use something that wasn’t needed for another medical purpose, that would be an advantage.”
“When you piece together a splitter, it creates a lot of dead space in the air circuit,” she explained. “It’s harder to exchange air when you’re moving all that dead space. As I realized the U.S. might have to ration ventilators, it was potentially worthwhile to spend the couple of weeks of calm we had to produce a splitter that would solve the dead-space problem, would be easy to use, and wouldn’t require a medical supply we would be competing for.”
INTERDISCIPLINARY COLLABORATION + SPEED = SOLUTION
“I came home after seeing my first COVID patient in the emergency department on a Friday and said to Ryan, ‘I think you need to build me something with the 3D printer.’”
By the end of the weekend, he had created a functional model on the family’s 3D printer. Three days of testing with pulmonologist Antine Stenbit, M.D., Ph.D., followed.
“We then modified it, pulling in more doctors and engineering work groups with collaborators at University of South Carolina and Clemson University to refine and retest,” Farris said.
“Designing the device was fairly simple. I could model it from beginning to end in a half-hour or so. It took a couple of days of back and forth and printing different revisions to fit right. There are ISO standards for respiratory connecting parts, and I was trying to do it with calipers. That was difficult, taking three to four hours to print each part. Then Dr. Stenbit would give us a yes/no whether it worked. Eventually I bought the ISO standards just to be sure I was printing it correctly. At that point, we got a good fit and it worked.”
Having printed the splitter on the family’s 3D printer, Farris then took on the problem of scalability. “Polylamide (PLA) is the common material used in printing toys and small products on home printers,” he said. “We needed something stronger — material that would meet medical device standards. An ICU worker and a friend volunteered their industrial 3D printing and manufacturing experience. At the same time, I spun up on research papers, seeing what others were using for research devices. Eventually we settled on a type of nylon called PA-12 to print the part. We also considered medical-grade polycarbonate, but PA-12 could be printed in batches of 1,000, whereas the polycarbonate was a much slower process. All together, it took four iterations for the parts to seal correctly.”
SPRINTING TOWARD PRODUCTION
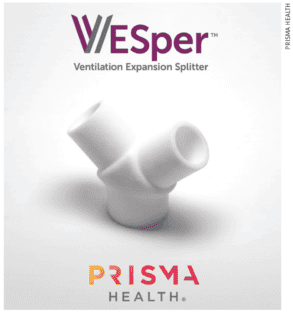
“Soon after, through the Prisma network, we were able to hook up with Clemson’s 3D printing and reverse-engineering lab, which has an industrial 3D printer that could print PA-12 nylon, and produce our prototype parts locally,” Farris said. “Then we searched for the Hewlett Packard machines that print 1,000 parts at a time. We found large, certified producers that make existing medical parts, and were willing to help.”
At this point it started to get serious. Prisma Health rapidly hammered out the details with its partner, Johnson & Johnson Ethicon.
“We’re limited to emergency use of the VESper for only two patients,” Dr. Farris said. “As I said, ventilators have been split up four ways in situations like the Las Vegas shootings, but those victims had healthy lungs, and this is purposed for potentially critically ill patients. A ventilator can produce up to 300 liters per minute of air flow, and a patient needs up to 30 liters per minute in total. A normal ICU ventilator is capable of producing that flow. But you can’t just take a ventilator and magically split it two, three, four ways and have it work. You have to match patients with similar lung compliance and ventilator settings, and control pressure so they get appropriate total volume for their size. That way, if one person starts to get worse, you can protect the other person, because no matter what, both get the pressure they need.”
ADVICE FOR INVENTORS
For engineers and doctors fighting to get emergency inventions to production, the couple has valuable advice. “Be aware of what’s already available,” Dr. Farris said. “Many people working in parallel on different designs is useful, but can be reinventing the wheel. Several different ventilator splitters have been designed in the last two or three weeks around the world due to COVID, so it helps to know how your goals are different from the others. Pull in collaborators with different skillsets because they will think of issues you haven’t, and that helps you come up with a better product.”
“Avoid issues down the road by studying what’s out there and adapt it to your specific needs,” her husband added. “That’s what helped us through the process.”
“Having a partnership with a human simulation can be really helpful,” Dr. Farris continued. “In my role with the Greenville HealthCare Simulation Center, we were able to use resources for testing the iterations of the device on simulations of a hospital environment, and could have a therapist come with a ventilator to try it out. Simulation centers are used a lot for staff training, medical students, and nurse education, but many of these simulation centers are interested in R&D roles, so don’t hesitate to reach out.”
The VESper went from prototype to production with stunning speed — 11 days from prototype to FDA emergency-use authorization. Asked for her thoughts on this remarkable effort, Dr. Farris paused. “I wish it weren’t necessary. It’s inspiring to see people come together, people working from home, pitching in their free time, seeing the best of their capabilities. But I wish we didn’t need any of it.”
MATH FOR A CRISIS MOMENT
We’ve all seen the red circles, spreading across the globe on the Johns Hopkins coronavirus map. Since the early days of the pandemic, anyone on Earth with an internet connection has been able to easily track the number of cases in real time, and pinpoint their locations.
Lauren Gardner, Ph.D., associate professor in the department of civil and systems engineering, and co-director of the Center for Systems Science and Engineering at Johns Hopkins University, created this relatable, crystal-clear, and up-to-date dashboard.
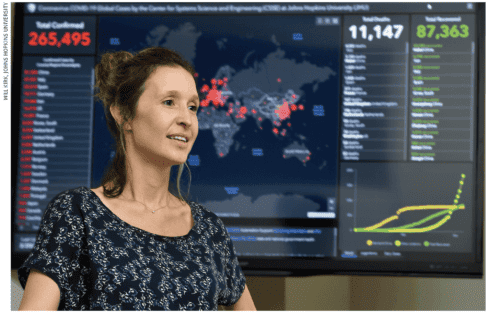
“Our data collection, reporting, and validation process has changed over time,” Dr. Gardner said. “It started out fully manual. It was just two of us, with data entry being led by Ph.D. candidate Ensheng Dong. However, now we have a lot of additional support from the Johns Hopkins University Applied Physics Lab, and a team at Esri, who has the mapping software and helps manage the platform. Now the entire process is mostly automated. There’s a systematic anomaly detection system in place that tracks and alerts us to increases and decreases in the case reports that we are automatically collecting from various sources, so we can more efficiently check those.
“Additionally, and critically, there are millions of eyeballs on this dashboard all the time. So if we’re off on a number, people reach out and contact us very quickly. We have received thousands of emails telling us about new cases, or when there are discrepancies in our case reporting, which we can quickly correct. It’s an ever-evolving process.”
Dr. Gardner noted that additional teams (at JHU) help her team manage the media and communications around its work.
Remarking on response to the map, she said, “I think its value is clearly evidenced by its popularity. We get over a billion hits on the dashboard per day. It’s used all over the world, by everyone from the general public to the U.S. Department of State. There was clearly a huge gap in the need to provide freely accessible, real-time data about such an evolving situation that we filled, which is critical to moving forward.”
Dr. Gardner’s interests and efforts have returned to mathematical modeling around COVID-19. “We are now doing real-time risk assessment of what’s going on in the U.S., aiming to feed these results back to policymakers to help identify the U.S. counties that we should be worried about ‘tomorrow.’ It’s important for us to get back into policy support for decision-making, because we can do it.”
“WE ARE NOW DOING REAL-TIME RISK ASSESSMENT OF WHAT’S GOING ON IN THE U.S., AIMING TO FEED THESE RESULTS BACK TO POLICYMAKERS TO HELP IDENTIFY THE U.S. COUNTIES THAT WE SHOULD BE WORRIED ABOUT ‘TOMORROW.’ IT’S IMPORTANT FOR US TO GET BACK INTO POLICY SUPPORT FOR DECISION-MAKING, BECAUSE WE CAN DO IT.”
– Lauren Gardner, Ph.D., creator of the Johns Hopkins University coronavirus map
On April 17, 2020 the JHU coronavirus map updated with a tool that drills down to U.S. county by county, real-time statistics. See https://coronavirus.jhu.edu/us-map.
“COVID-19: STEM Strikes Back” was written by Seabright McCabe, SWE Contributor. This article appears in the 2020 spring issue of SWE Magazine.
Read more from the 2020 spring issue of SWE Magazine:
- Feature: Toward More Accessible Work Environments
- Feature: Engineering for Good
- Feature: Inclusive Design for Living Longer
- Feature: Women Engineers You Should Know
- SWE Forum: From Congressional Visits to the “New Normal” Brought by COVID-19
- Opening Thoughts: Access: A Matter of Human Rights
- News & Advocacy: Momentum, Authenticity, and Pivoting: The State of Women in Politics
- News & Advocacy: Visiting Congress During a Global Health Crisis
- News & Advocacy: People
- Career Pathways: Shelter-at-Home Orders Put Spotlight on Disability Accommodations
- President’s Note: Joy and Relevance in the SWE Mission
- Life and Work: Is Sitting the New Smoking?
- Reinvention: From Fixing up My Home to Helping Others Construct Theirs
- Media: Invisible Women: Exposing Data Bias in a World Designed for Men
- Viewpoint: Then and Now: Personal Reflections on Accessibility
- In Memoriam: Marta Kindya, 1946-2019
- Closing Thoughts: Community in Times of Crisis
- Scrapbook: Announcing a New Arrival